Dear patient the information provided to you is based on the evidence-based literature available and our vast clinical experience with the intention of providing insights into the frozen shoulder, its symptoms and treatment available.
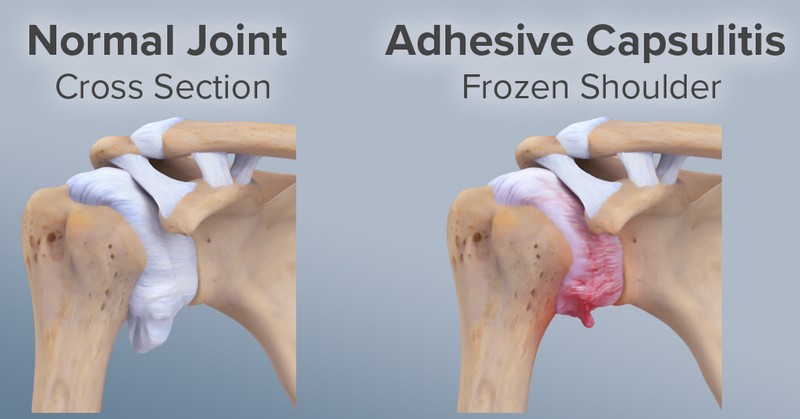
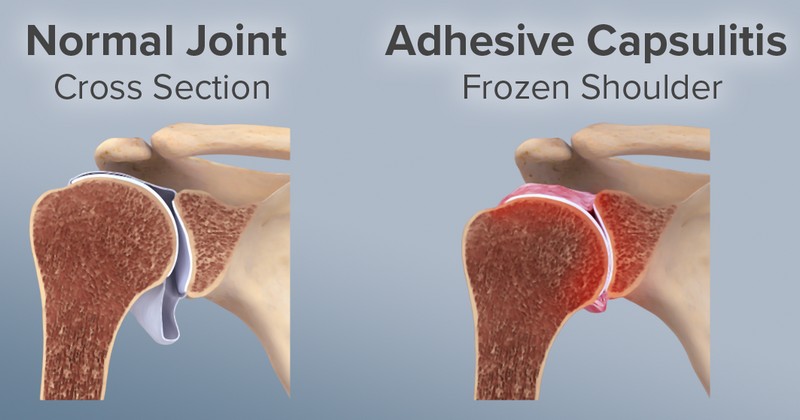
Frozen shoulder, also called adhesive capsulitis, causes pain and stiffness in the shoulder. Over time, the shoulder becomes very hard to move.
After a period of worsening symptoms, frozen shoulder tends to get better, although full recovery may take up to 2 years in certain patients.
Physiotherapy, with a focus on shoulder movements, is the primary treatment recommendation for frozen shoulder.
Frozen shoulder most commonly affects people between the ages of 40 and 60, and occurs in women more often than men. In addition, people with diabetes are at an increased risk for developing frozen shoulder.
In frozen shoulder, the shoulder capsule thickens and becomes stiff and tight. Thick bands of tissue — called adhesions — develop. In many cases, there is less synovial fluid in the joint.
The hallmark signs of this condition are severe pain and being unable to move your shoulder — either on your own or with the help of someone else. It develops in three stages:
Stage 1: Freezing
In the “freezing” stage, you slowly have more and more pain. As the pain worsens, your shoulder loses range of motion. Freezing typically lasts from 6 weeks to 9 months.
Stage 2: Frozen
Painful symptoms may actually improve during this stage, but the stiffness remains. During the 4 to 6 months of the “frozen” stage, daily activities may be very difficult.
Stage 3: Thawing
Shoulder motion slowly improves during the “thawing” stage. Complete return to normal or close to normal strength and motion typically takes from 6 months to 2 years.
Cause
The causes of frozen shoulder are not fully understood. There is no clear connection to arm dominance or occupation. A few factors may put you more at risk for developing frozen shoulder.
Diabetes, hypothyroidism, hyperthyroidism, Parkinson’s disease, and cardiac disease.
Immobilization – Frozen shoulder can develop after a shoulder has been immobilized for a period of time due to surgery, a fracture, or other injury.
Diagnostic tests
X-rays may show other problems in your shoulder, such as arthritis.
Magnetic resonance imaging (MRI) create better images of soft tissues. They are not required to diagnose frozen shoulder, however, they may help to identify other problems in your shoulder, such as a torn rotator cuff.
Treatment
Occasional painkillers and physiotherapy stretching exercises will ease the condition in majority of patients.
Stronger pain relief is usually only used for a short time because it can cause side effects.
Physiotherapy for frozen shoulder
Physiotherapy can help you get movement back in your shoulder.
A physiotherapist will decide the number of sessions you need. The exact number depends on how your shoulder responds to treatment.
The physiotherapist will first check how much movement you have in your shoulders.
Treatments from a physiotherapist include:
- stretching exercises
- strength exercises
- good posture advice
- pain relief advice
Most frozen shoulders get better within 12 to 18 months.
Surgery. Surgery for frozen shoulder is rare, but if pain is disabling and quality of life is disturbed, arthroscopic capsular release and subacromial decompression is performed which will give good results.
You may get a mix of these treatments depending on how painful and stiff your shoulder is.
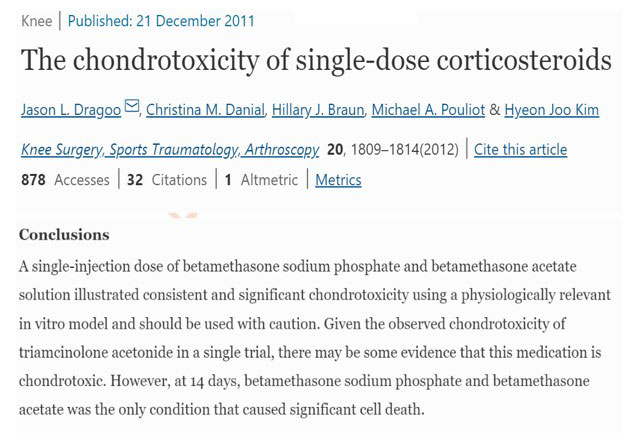
WE DON’T ADVISE INTRAARTICULAR STEROIDS BECAUSE OF ITS SHORTLIVED BENEFITS AND ASSOCIATED COMPLICATIONS
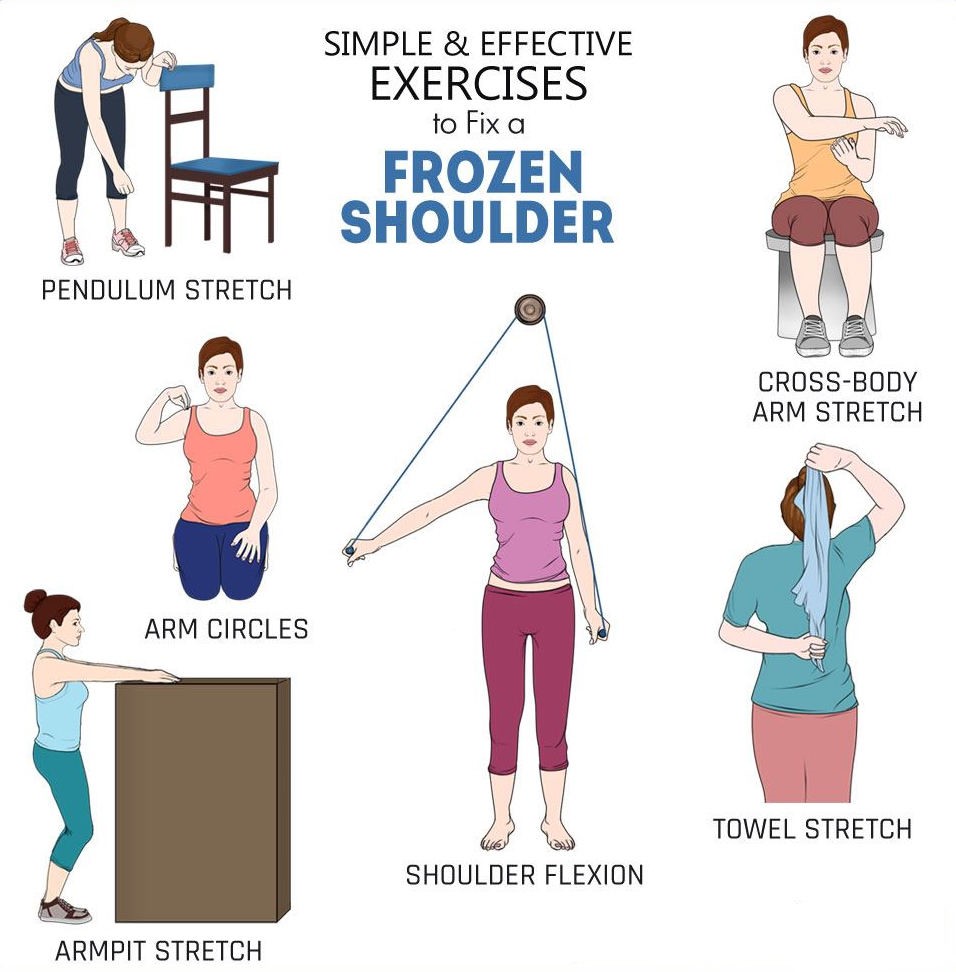
Apart from these it is suggested to consult physiotherapist for resistance band exercises



Follow us